Saturday, June 26, 2021
OBGYN books for Houseman (HO)
Books recommended
Friday, June 25, 2021
EPR June 2021 OSCE
Great thanks to those who contributed to the list, and hope you guys will be able to pass the exam with flying colours!
Good luck
EPR June 2021 (IMU)
1. IUGR/SGA ddx
- - Small gestational age. 39th GW (counsellig)
2. Nephrotic syndrome:
- Facial puffiness (hx taking, data intepretation, tx
3. Megaloblastic Anemia
- -PBF: hypersegmented neutrophil.Vit B12 deficiency
4. Suturing
- 3 simple interrupted suture)
5. ECG placements.
- Intepret Ecg ventricular tachycardia. how to use cardioversion?
6. Supraspinatus tendonitis
- Shoulder physical examination.
- Xray- Supraspinatus tendonitis,tx
7. compartment syndrome,
- - Knee (full leg cast) tx
8. Cataract
- - Blur vision( hx taking) visual acuity. Pupillary exam
9. PE neuro
- Focal seizure (adult) hx taking, dx, two drugs
10. Pott's disease
- Radiology (pulmonary tb, ddx)
11. Alcohol abuse (hx taking) tx
12. Breaking Bad news
- Patients family requesting not to disclose patient's terminal condition. Hepatocellular carcinoma
13. Hyperemesis gravidarum
14. ABCDE + ETT displacement
- Correct asymmetrical lung intubation
15. Male urinary catheterisation
16. Neonatal jaundice,
- test for further Ix, graph chart for tx. ABO hemolysis? Physiological jaundice?
Sunday, June 6, 2021
Hypertension in Pregnancy
Hypertension in Pregnancy
Differences
- Chronic HPT: <20wks dx or beyond 6wks postpartum
- Gestational HPT/ pregnancy induced hypertension (PIH without proteinuria) / Preeclampsia(PIH with proteinuria) / Eclampsia (PIH with convulsion): > 20wks dx
- Chronic HPT with superimposed preeclampsia : PE in women who have pre existing hypertension. Include: worsen HPT, proteinuria, non-dependant oedema.
Pathophysio of preeclampsia
Found this video on youtube which is quite useful in helping to understand about Preeclampsia. Enjoy!
complications
Need for delivery when
Postpartum monitoring
Management
- diastolic BP 90-100, no proteinuria
- Mx:
- rest at home with daily BP and urine check by community midwife
- once or twice weekly Day Care Unit attendance for BP and CTG check
- delivery by term or sooner
- diastolic BP 100-110 or less if complicated by proteinuria
- Mx:
- tx in hospital, daily ur albumin, 4hrly BP
- check fluid balance, amount of oedema
- weekly weight
- Daily CTG
- Meds: labetalol 100mg TDS max 300mg 6hrly , T. methyldopa 250mg QID to max 3g/d
- deliver 38wks or sooner
- almost like severe PE Mx
- proteinuria>3g/L
- BP>160 systolic
- BP>110 diastolic with no BP > than 160/110 with no proteinuria
- oliguria (<400ml/24hrs)
- presence of Impending Eclampsia
- Mx:
- Tx in hospital
- Observation and meds like PIH
- check for
- reflex, clonus
- opthal
- LFT, PLT
- quantitative proteinuria daily
- Delivery by 36 wks or sooner
- Aim to reduce to diastolic 90-100mmHg
Key Points:
2nd trimester: 13-26
3rd trimester: 27-EDD(40)
Saturday, June 5, 2021
shoulder dystocia
Shoulder Dystocia (SD)
1. Definition
2. Risk factors
3. HELPERR
4. BE CALM
5. Complications
6. Prevention
** HELPER, BE CALM
Definition:
- unanticipated obstetric emergency which requires early recognition and rapid intervention
- refers to a situation where after delivery of the head, the anterior shoulder of the fetus becomes impacted on the maternal pubic symphysis, or (less commonly) the posterior shoulder becomes impacted on the sacral promontory.
RIsk factors:
- maternal
- maternal obesity
- small maternal stature
- GDM
- previous SD
- IOL
- prolong stage 1 and 2 of labour
- augmentation of delivery
- fetal
- macrosomic
- instrumental delivery
When SD occurs
Adapt BE CALM
Complications:
- Fetal:
- Brachial Palsy, Brachial plexus injury,
- fracture of clavicla and humerus
- cerebral hypoxia- d/t delay of delivery (should deliver within 5minutes once baby head out)
- Ischemic encephalopathy
- Cerebral palsy
- maternal:
- vaginal and perineal laceration
- 3rd and 4th degree tears
- postpartum hemorrhage
- uterine rupture(rare)
Preventions:
Friday, June 4, 2021
obstetric emergencies
Obstetric emergencies
Cord prolapse
Definition:
1. overt umbilical cord presentation: umbilical cord lies infront of the presenting part and the membranes are intact.
2. Overt umbilical cord prolapse: when the umbilical cord lies in front of the presenting part and the membranes have ruptured.
3. occult umbilical cord presentation/ prolapse: the umbilical cord lies trapped beside the presenting part rather than below it
Risk Factors:
1. non- iatrogenic : fetal abnormal lie/malpresentation/breech, polyhydramnios, multiple pregnancy, prematurity, IUGR/SGA, high presenting part.
2. iatrogenic: Amniotomy, placement of cervical ripening balloon catheter, vaginal manipulation of fetus with ruptured membranes.
3. External cephalic version.
- complication: birth asphyxia (d/t cord compression or vasospasm)
Management:
- call for HELP! arrange OT!
- continue CTG
- relieve cord compression
- using position: knee to chest position/ Tredelenburd position/ cephalad gravitation
- help decrease blood flow, avoid fetal asphyxia and acidosis
- cord vasospasm -which caused by exposing to surrounding
- no oxytocin, only tocolytic agent: terbutaline 0.25mcg
- ***do not push back the cord
- *** no amniotomy
- if you are doing VE: gentry push fetal head upwards, away from maternal pelvis (to relieve cord compression). use suprapubic pressure to keep fetus away from pelvis.
- insert 500ml warm water in to urinig
***1. discontinue oxytocin
- administer tocolytic agents(s/c terbutaline 0.25mcg stat) if there are fetal brady
- minimize excessive handling of the umbilical cord
- if cord is outside, gently wrap the exposed cord with warm gauze.
2. never replace cord into uterus (causes vasopasm and fetal hypoxia)
3. DONT remove examining fingers.
4. doppler ultrasound: to detect occult cord presentation
- deliver fetus ASoon/safeAP and
- instrumental delivery if favourable
- breech extraction if favourable
- deflate bladder before peritoneal entry of C-section
Uterine rupture:
Uterine Dehiscence
Causes:
Types:
1. completely rupture: extend through myometrium and serosal peritoneum
2. incomplete rupture: overlying peritoneum still intact, includes scar dehiscence
Symptoms:
- PV bleeding
- suprapubic pain and tenderness
- shock
- undetectable fetal heart beat
- CTG sudden cariable/late deceleration before onset of fetal bradycardia
- easily palpable fetal body parts
- loss of station
- cessation of uterine contraction
Diagnosis via
- protrude amniotic sac
- hematome
- endometrial/myometrial defect
- intraperitoneal fetal part
- hemoperitoneum/ free fluid
Management
- Intensive resus
- emergency laparotomy
- hysterectomy unless there are reasons to preserve uterus
- rupture repair
- Broad spectrum antibiotic
- cephalosporin
- flagyl (metronidazole)
- Adequate post operative care
POST PARTUM HEMORRHAGE
DEFINITION:
Mx:
- bleeding >1.5L --> can be seen in drop of BP
- tachycardia >100bpm
- 1st
- active resus
- uterine massage
- IM symptometrine
- 1ampule pitocin (max: 80u)
- IM hemabate
- then IVI 40u pitocin maintanence
Dose | Oxytocin | Ergometrine | 15-Methylprostaglandin F2 |
Dose and route | IV : Infuse 20 IU in 1L IV fluids at 60 drops/min | IM or IV (Slowly) : 0.2mg | IM: 0.25mg |
Continuing dose | IV : Infuse 20IU in 1L IV fluids at 40 drops.min | Repeat 0.2mg IM after 15 min If required, give 0.2mg IM or IV (slowly every 4 hours) | 0.25mg every 15 minutes |
Maximum dose | Not more than 3L of IV fluids containing oxytocin | 5 doses (Total 1.0mg) | 8 doses (Total 2mg) |
Precautions/ Contraindications | Do not give as an IV bolus | Avoid in pre-eclampsia, hypertension, heart disease | Bronchospasm (CI in Broncial Asthma) |
Tuesday, June 1, 2021
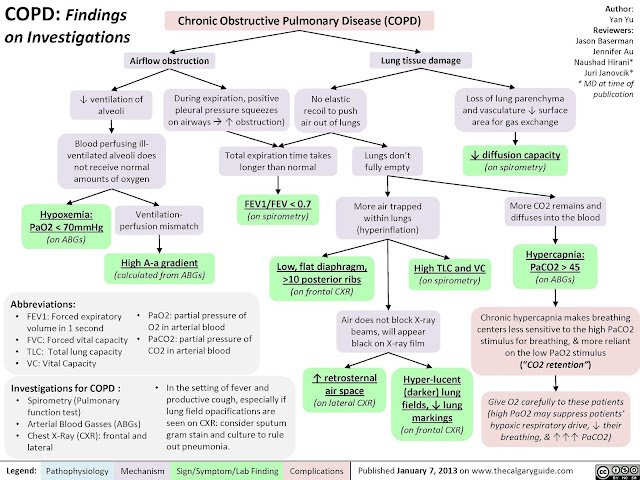
COPD
COPD
- pathophysio
a preventable and treatable respiratory disorder largely caused by smoking, is characterised by progressive, partially reversible airflow obstruction and lung hyperinflation with significant extrapulmonary (systemic) manifestations1 (Level II-2) and comorbid conditions2 (Level II-3) all of which may contribute to the severity of the disease in individual patients.
due to a mixture of small airway disease (obstructive bronchiolitis) and lung parenchymal destruction (emphysema), the relative contributions of which vary from individual to individual. Airflow limitation, associated with an abnormal inflammatory reaction of the lung to noxious particles or gases, the most common of which worldwide is cigarette smoke, is usually progressive, especially if exposure to the noxious agents persists.
diagnosis and severity assessment of COPD, a post-bronchodilator FEV1 /FVC ratio of < 0.70 and post-bronchodilator FEV1 measurement, respectively are recommended.
The pathological changes in COPD,
which include chronic inflammation and structural changes resulting from repeated injury and repair - -
- due to inhaled cigarette smoke and other noxious particles,
- are found in the proximal airways, peripheral airways, lung parenchyma, and pulmonary vasculature.
The chronic inflammation in COPD is
- characterised by
- an increase in the numbers of neutrophils (in the airway lumen),
- macrophages (in the airway lumen, airway wall, and parenchyma), and
- CD8+ lymphocytes (in the airway wall and parenchyma).
- differences in physiological changes, symptoms and response to treatment
- These pathological changes lead to
- mucus hypersecretion,
- expiratory airflow limitation
- with dynamic small airway collapse causing
- air trapping and lung hyperinflation,
- gas exchange abnormalities, and
- progressive pulmonary hypertension t
- hat may lead to cor pulmonale.
- There is further amplification of the inflammatory response in the airways during exacerbations,
- which may be triggered by bacterial or viral infections or
- by environmental pollutants.
- In general, the inflammatory and structural changes in the airways increase with disease severity and persist on smoking cessation.
PE:
Physical signs of airflow limitation and air trapping (barrel chest, loss of cardiac and liver dullness, prolonged expiration, reduced breath sounds)
Ix
Signs symptoms of exacerbation
noctural cough : why?
- Patients with nocturnal asthma symptoms may have greater nighttime activation of inflammatory cells and mediators, lower levels of epinephrine and increased vagal tone

ddx:
- bronchial asthma
- CHF
-pulmonary edoema,
pneumonia
-bronchiectasis
-pulmonary vascular disease
Outpatient management
- bronchodilators: beta agonist(salbutamol 2.505mg)/ipratropium bromide
- corticosteroids (fev1<50 30mg per day for 1week)
Types of meds
- Acute exacerbation: doxycycline 100mg/ amoxycillin 500mg QID
- CAP: ampicillin_ azithromycin
- severe:
- wihtout beta lactamase inhibitor (piperacillin-tazobactam) /cefepime
- Gram positive:
- staphylo, strepto, pneumococci, tb: cloxacillin, penicillin g,
- gram negative:
- e coli, pseudomonas aeruginosa: aminoglycosides (gentamycin), cephalosporin(ceftriaxone), fluoroquinolones (ciprofloxacin)
- tonsilitis: amoxycillin
- meningitis: ceftriaxon + ampicillin