HPB = Hepatobiliary
Anatomy of HPB
Common classifications used in HPB
1. Ranson criteria
2. Mirrizi classification
biliary colic -> acute cholecystitis -> acute cholangitis, pancreatitis, gb empyema and gangrenous gb
presentation of each spectrum
Causes of obstructive jaundice
painless vs painful jaundice
- Painful obstructive jaundice is usually related to gallstones, while painless obstructive jaundice tends to be related to tumours.
Q1: If patient came with features of ascending cholangitis, what Investigation you would like to order
- FBC - to monitor TWC, PLT.
- low platelet: sepsis induces/ severe sepsis that causes coagulopathy
- BUSE - urea, creat monitoring
- hyperbilirubinemia can cause hepatorenal syndrome and renal impairment
- severe sepsis that causes organ failure : kidney failure
- LFT: TB, kiver enzymes and albumin level
- especially ALP and direct bilirubin that can help determin if there are any obstructive jaundice
- ABG: any acidosis or resp failure
- CXR first, as we can use it to rule out perforated viscus
- unless obvious jaundice, so less likely perforated PUD
Q2: why we need ultrasound HBS for ascending cholangitis?
- to rv CBD(common bile duct) size, and any dilatation
- any stone present- if there's obstruction , might need urgent intervention to relieve obstruction
- sometimes stone cant be seen as obscured by bowel gas.
- stone is usually in distal CBD - the narrowest part
- and it is at the back of duodemun
- usg wave cannot go through gas
- To rule out liver abscess
- as the presentation of liver abscess is the same: RHC pain, fever and jaundice
Q3: normal size of CBD?
- 3-5mm
- >8mm considered dilated (usually we use >10mm or 1cm as dilated)
Q4: why do we need to rule out liver abscess urgently?
- if huge liver abscess need to drain urgently.
- gold standard tx: percutaneous drainage and antibiotic
- otherwise it will rupture and cause peritonitis --> severe sepsis --> mortality
Q5. if found out patient have ascending cholangitis secondary to choledocholithiasis, how would you manage?
- resuscitate and stabilize the patient first with ABC
- Airway
- Breathing
- Circulation
- insert branula + blood for Ix and blood culture
- fluid resus
- antibiotics
- analgesia
Q5a. what are the choice of antibiotics use for the pt above?
- HBS common organism are
- function of liver: it uses portal circulation,
- it collects blood from gut - all the guy -> return back to liver
- therefore in the GI tract, mainly organism gram negative and anaerobes
- also called BROAD SPECTRUM of negative organisms
- so we need at least 3rd generation cephalosporin
- eg: cefobid / cefoperazone
- to cover anaerobes: metronidazole
Q6. after analgesics what can we do for patient with ascending cholangitis and in pain?
- if Stable, we can try ERCP to remove the stone . if unable to do so we will put stent to drain the obstruction
- ERCP needs sedation, and prone position. therefore difficult to maintain airway
- If patient is unstable , the option is PTBD
Q7. when to do cholecystectomy?
- once sepsis is resolved
- stone not cleared through ERCP
Q8. How do you tell which liver segment was it from a CT scan?
Anatomy of liver :
note that 2 is beside 4a, 3 below 2 and 4b is below 4a
upper segment at right side is segment 7,8
and lower right is segment 6 and 7
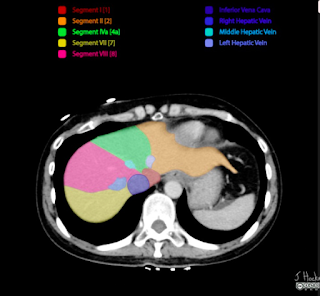 First you can check the segments from identifying the hepatic veins. As shown in diagram above, left hepatic vein separates segment 2 and 4a, then the middle hepatic vein for segment 4a and 8, right hepatic vein for segment 8 and 7
First you can check the segments from identifying the hepatic veins. As shown in diagram above, left hepatic vein separates segment 2 and 4a, then the middle hepatic vein for segment 4a and 8, right hepatic vein for segment 8 and 7Then as you scroll down the ct scan, you will see the portal vein (left branch). the portal vein separates the liver to the left(segment 2 and 4a) and right side (segment 7,8) . below the portal vein emerges segment5
When you can see the right branch of portal vein, it also indicates that on Left (segment 4b, and segment 3), on its right is segment 5 and segment 6












